From adherence to outcomes:
The Patient Support Programme of the future
Published May 16, 2024
- Life Sciences

Patient Support Programmes (PSPs) have traditionally provided a static type of support.Whether the focus has been for example patient education or adherence, the engagement through the support programme has often been ‘one-way’. Even when technology solutions are used, such as SMS-reminders, the set-up has been structured to deliver a non-personalised service without taking advantage of the direct link with the patient.
However, there is a new generation of PSPs showing the way by creating an integrated environment where human engagement, technology and data co-exist in symbiosis.
This new generation of PSPs are able to command a much more strategic role in an evolving pharma environment and new business models; the PSP of the future:
- Leverages technology to deploy scalable and personalised human engagement
- Captures real world data on health outcomes, establishing an evidence and insights engine that can feed innovative commercial arrangements
- Captures experience, operational and other patient data feeding a continuous improvement loop
- Creates a touch-point with patients that has the potential to bend the pharmaceutical value chain, drive category leadership, and turn the vision of patient-centricity into practice
A new generation of patient support
Companies that fail to see the broader potential of patient support, risk being reduced to a product provider, at mercy of rebate and discount conversations, rather than a partner in healthcare that find alignment with stakeholders around common objectives for patient and system outcomes.
On the other hand, if you are starting to think about how patient support can give you that strategic advantage, you are early enough to get ahead of a lot of your competition. While at the same time, you have the opportunity to learn from some of the first-movers in this space.
What is a PSP as an integrated healthcare service?
Patient support in the form of integrated healthcare services consists of a care service core, where human engagement co-exists with digital, connected care elements. This service core is powered by two data loops.
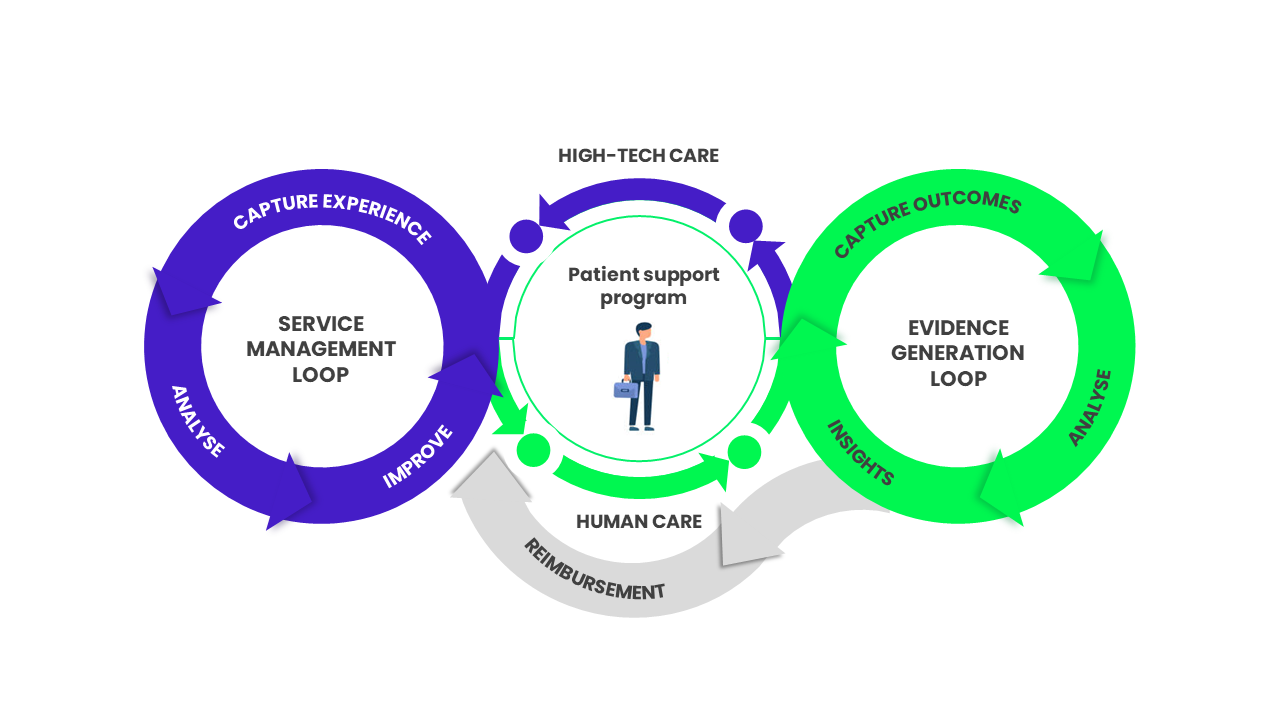
The first is focused on operational and experience data. By capturing a combination of operational data (e.g. time on the phone with nurse) and experience feedback data (e.g. was this easy for you? Did you get what you needed?) at the touch-point level, you are able to do three things:
- You can start to know your patients and their preferences, and segment your population accordingly. This is the cornerstone of scalable patient support
- You can continuously improve your operational efficiency by knowing how you are performing and what actually provides value to your patients
- You can allocate resources accordingly – both strategically as you evolve the service and operationally, serving the patients with the most need
The second data loop is focused on health and system outcomes to generate evidence. The digital interface with the patients creates a touchpoint that allows you to capture health outcomes data more seamlessly than, for example, traditional in-clinic questionnaires.
For instance, imagine a daily prompt that asks the patient how they are feeling and based on the answer can suggest different interventions. The suggestions provide value to the patient and help him/her manage their condition. While the prompt questions capture valuable Quality of Life (QoL) data.
This kind of data directly from the patient can then be combined with other data sources, such as weather, location, physical activity, or pollen, that are all captured latently through the smart phone.
The combination of data sets creates both valuable insights on how the patient is doing in real time to support interventions. For example, in COPD this data together with predictive analytics could foresee acute exacerbations and put in place mitigating activities or alerts. Alongside this, he data also provides the potential foundation for outcomes-based reimbursement and other innovative commercial models.
By building these continuous data capture and improvement loops around a digitally enabled service offering, the PSP becomes a centrepiece of a new kind of offering.
How do I make it work?
The objectives and measures of success should be relevant to patients and stakeholders (adherence is really a means to a goal). Alongside co-creation and iterative development, defining the right goals and KPIs are critical to the success of a patient support programme. There are several reasons why this is so important, but when it comes to more innovative programmes that rely on, for example, data capture and behaviour change, the way KPIs and goals are set up can enable or limit what you can and cannot do.
Two examples:
- Net Promotor Score (NPS), although a commonly used experience metric, has its limitations from a compliance perspective in a patient support setting*
- Adherence, although an important operational, as well as business KPI, can limit the type of data you can capture and analyse
Therefore, it is important that patient and payer relevant outcomes are front-and-centre.
A sure way of creating a failed PSP is to develop it in isolation – co-creation is key.
The saying “don’t overestimate what you can do in the short-term and underestimate what you can achieve in the long-term” is very apt for this kind of undertaking.
A well-designed PSP can have profound impact, but it will take time to materialise and meet all of its objectives. Designing and launching a programme of this scale is completely contingent on having an iterative approach to scale.
Co-creation is crucial to understanding the highs and lows of your designed service from the perspectives of those who are either served by it or will be key to delivering it.
The dream of a fully scaled PSP can be realised if given the time to optimise the offering and overcome obstacles which arise during implementation.
Remember the importance of community and the human touch – personalised through technology, human engagement is what makes a PSP powerful.
The most successful PSPs have a human care component and several studies show the vast benefits that this has over ‘digital only’ approaches.
However, human care can also be an obstacle to scale and practical implementation as it is also cost intensive.
Having a digital element to the patient support that enables the human care and allows for data capture and subsequent personalisation of the level of human care a specific patient might need is critical.
Studies of the hugely successful Abbvie Cares PSP found that personalised services such as ‘Care Coach Calls’ (calls by trained nurses to patients for training and education) increased retention by 77%, and increased patient adherence and persistence.(1)
A common pitfall is designing a wonderful service that cannot be scaled. Integrate scale into the design process from the start and make sure your PSP can grow and evolve over time.
Patient support programmes often run into the issue of scale. Through our experience, there are three factors to think about to avoid the scalability conundrum:
- Involve markets early and co-create solutions
- Use technology to enable human engagement and personalisation of support (more on this on the next page)
- Design for scale by creating a stable backbone, a platform, where features can be turned on and off depending on market and compliance environment
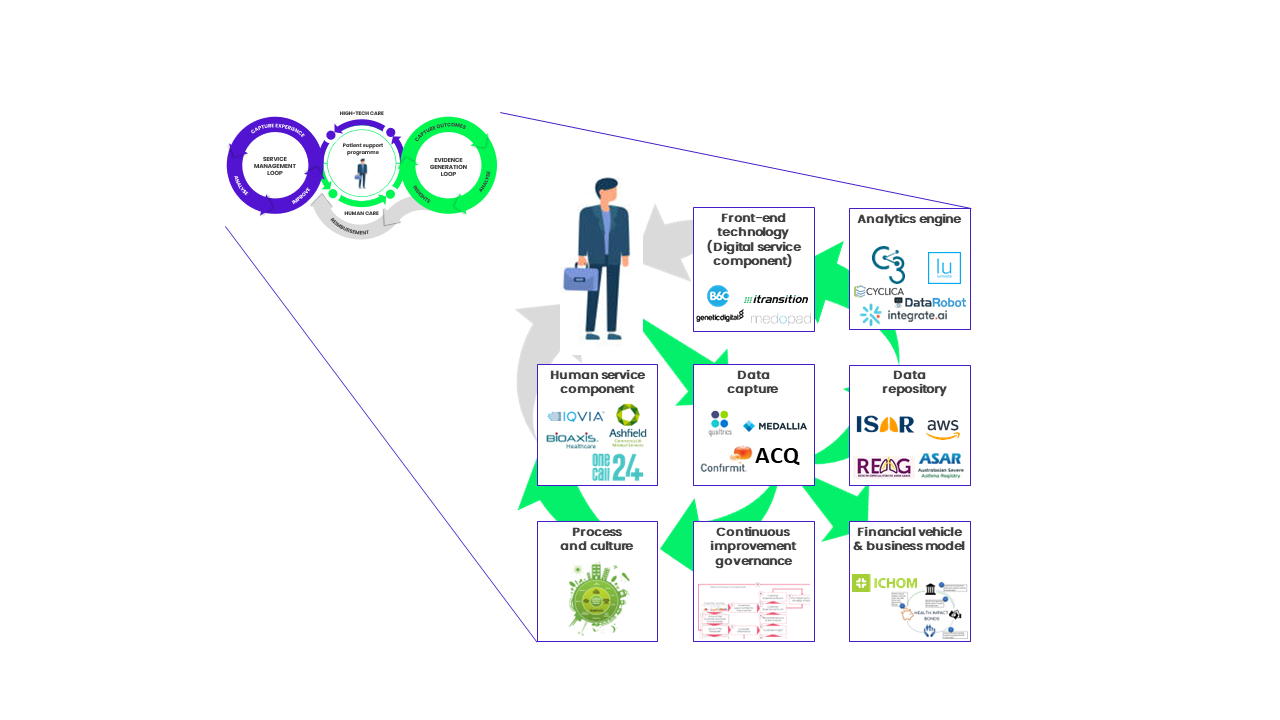
Not all that glitters is gold and not all new is innovation – often true innovation comes from combining existing technologies and solutions in new ways.
Another trap that pharma companies often fall into is thinking that innovation is restricted to service elements or technology features.
On the contrary, often the most disruptive innovation takes existing components and combines them in a new way.
For almost any challenge there are available technology options that can be acquired in the market. Pharma does not have to go and become a tech start-up.
In addition, solution and technology innovation must often be accompanied by commercial innovation.
Final Thoughts
PSPs can be so much more than just support. They can be the strategic centrepiece of new business models that reimagines the role that pharma plays in healthcare and patients’ lives.
We see companies moving away from traditional models of commercialising medicines in three different ways:
Some try to optimise the traditional model, using digital engagement and an enhanced understanding of the customer experience. PSPs in this context would probably not look vastly different from today. Digital will most likely be used, but may be confined to a website for example.
Another set of companies are evolving their offering without disrupting it. They are more frequently including services and solutions as part of their ‘holistic drug offering’. Instead of the much debated ‘beyond the pill’ we are probably looking at ‘around the pill’. Although technology may enable them in some ways, the full potential of the PSP is hampered by their position as a ‘value-add’ rather than a strategic platform.
A final set of companies are starting to think differently. Reimagining their business model and the role that they play in healthcare, these companies are introducing new thinking around outcomes, integrated care, and technology-drug-service combinations. In this context, PSPs will offer a vehicle to anchor the new business model around.
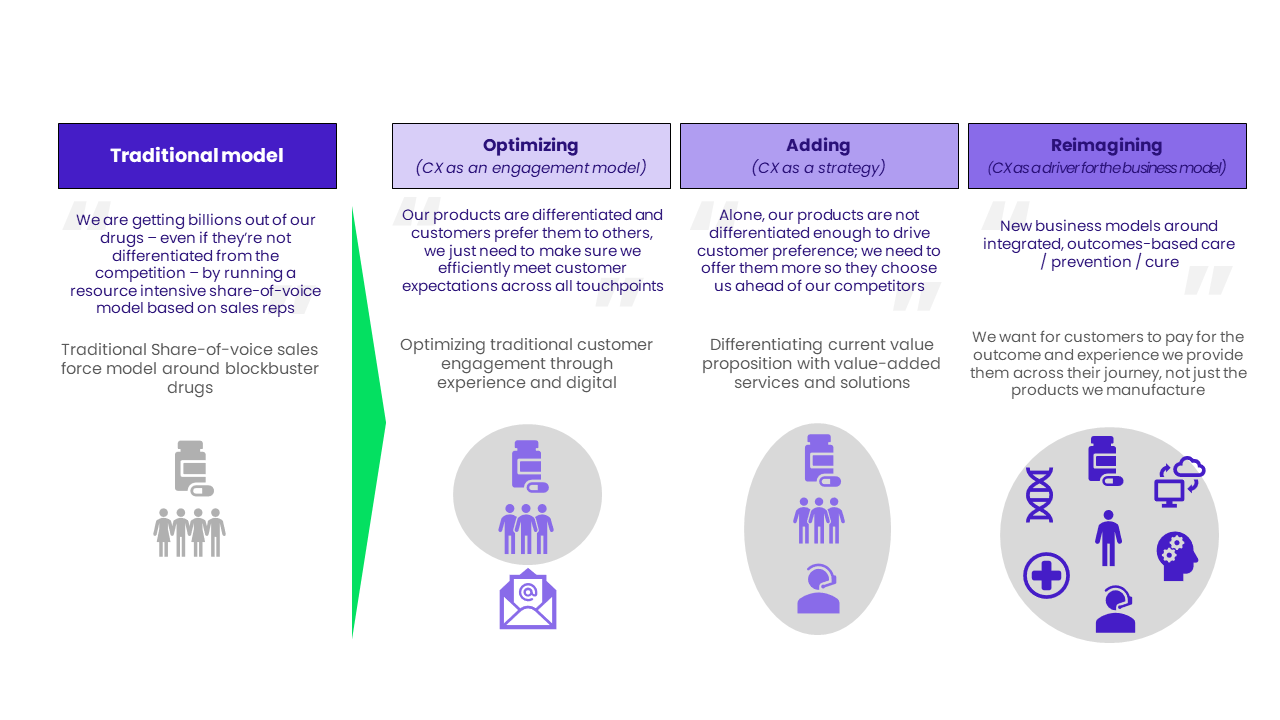
There is no ‘right answer’ and at Wavestone, we are supporting companies across all three of these models.
Ultimately, PSPs can do much more than just support adherence. And in fact, increasing evidence is showing this to be true. The new generation of PSPs that we see are improving health outcomes, improved work productivity and reducing total healthcare costs, while at the same time supporting their products through differentiation and competitive advantage. (2)
(1) Van den Bosch F, et al. Rheumatol Ther (2017) 4:85–96; Marshall JK et al., Clin Ther. 2018 Jun;40(6):1024-1032
(2) Rubin DT, et al. J Manag Care Spec Pharm. 2017;23(8):859–867; Ostor A, et al. EULAR 2018 AB1232
Author
-
Magnus Franzén-Rossi
Partner – UK, London
Wavestone
LinkedIn